Why SPMs May Offer Advantages Over Traditional Fish Oil
Jan 7, 2026
Why Specialized Pro-Resolving Mediators (SPMs) May Offer Advantages Over Traditional Fish Oil
Inflammation is a natural and necessary part of healing which comes in response to stress, injury, and infection. The problem arises when inflammation fails to properly resolve, leading to chronic, low-grade inflammatory states that underlie many modern diseases – such as obesity, atherosclerosis, hypertension, and chronic pain. For decades, omega-3 fatty acids — particularly from fish oil — have been promoted as a solution. But emerging research suggests that Specialized Pro-Resolving Mediators (SPMs) may represent a more targeted and physiologically appropriate approach. (1)
First let’s explore the basics….
What Are Fatty Acids?
Fatty acids are fundamental building blocks of fats (lipids) and are essential for:
Cell membrane structure and fluidity
Hormone and signaling molecule production
Energy storage and metabolism
Immune system regulation
Fatty acids are categorized by their chemical structure into saturated, monounsaturated, and polyunsaturated fats. Among polyunsaturated fats are two families humans cannot synthesize and must obtain from diet: omega-3 and omega-6 fatty acids.
Omega-3 vs Omega-6 Fatty Acids: What’s the Difference?
Omega-3s are generally considered anti-inflammatory or inflammation-modulating, especially when they are metabolized into downstream compound.
Key omega-3s include:
ALA (alpha-linolenic acid)
EPA (eicosapentaenoic acid)
DHA (docosahexaenoic acid)
They are found in foods such as fatty fishes like salmon, mackerel, and sardines, as well as walnuts, soybeans, eggs, flax and chia seeds.
EPA and DHA are especially important because they serve as precursors to SPMs, the molecules that actively turn off inflammation and initiate tissue repair. It’s important to note that conversion of ALA to EPA and DHA is inefficient, particularly in the context of insulin resistance, inflammation, nutrient deficiencies, or excess omega-6 intake.
Omega-6 fatty acids are not uniformly pro-inflammatory as traditionally thought. In fact, increased dietary intake does not consistently increase inflammatory markers in healthy adults. They are an essential component of the body’s inflammatory response system.
Key omega-6s include:
LA (linoleic acid)
AA (arachidonic acid)
They are found in foods such as corn, safflower and soybean oils, fish, egg, meat, and chicken, as well as many processed and ultra-processed foods.
Omega-6 to Omega-3 Ratio: Does It Really Matter?
For years, a 2:1 to 4:1 balance between omega-6 and omega-3 fatty acids was considered the gold standard. The prevailing theory was that lowering the omega-6 to omega-3 ratio would reduce inflammation, since omega-6 fats were thought to be inherently pro-inflammatory.
However, more recent evidence has begun to challenge this assumption. A growing body of research suggests that the ratio itself may have limited clinical relevance. Multiple trials have shown that increasing omega-6 polyunsaturated fatty acid intake—particularly linoleic acid—while keeping omega-3 intake stable does not worsen markers of inflammation or oxidative stress. (2)
What appears to matter more than the ratio is the total and absolute intake of omega-3 fatty acids. In particular, higher intakes of EPA and DHA have consistently (but not always) been associated with cardiovascular benefit.
Some clinical outcome studies have been shown to reinforce this point. Rather than focusing on reducing omega-6 intake, increasing EPA and DHA consumption is part of what drives a meaningful reduction in cardiovascular disease risk. In fact, the 2025 American College of Cardiology scientific statement reports that for every additional 1 gram per day of EPA plus DHA, the risk of myocardial infarction is reduced by 9%, total coronary heart disease by 7%, and overall cardiovascular events by 5.8%. (3)
Overall, there are significant global insufficiencies in omega-3 levels with many countries having suboptimal range (less than 5.4%). A study published in Lipids in Health and Disease in August 2025, analyzed over 590,000 dried blood spot (DBS) samples from around the world to assess omega-3 fatty acid status and omega-6 to omega-3 ratios. The graph below demonstrates how the United States is generally deficient. The natural thought is that we should just increase our omega-3 intake via supplementation. However, this might not be enough in chonic illness.
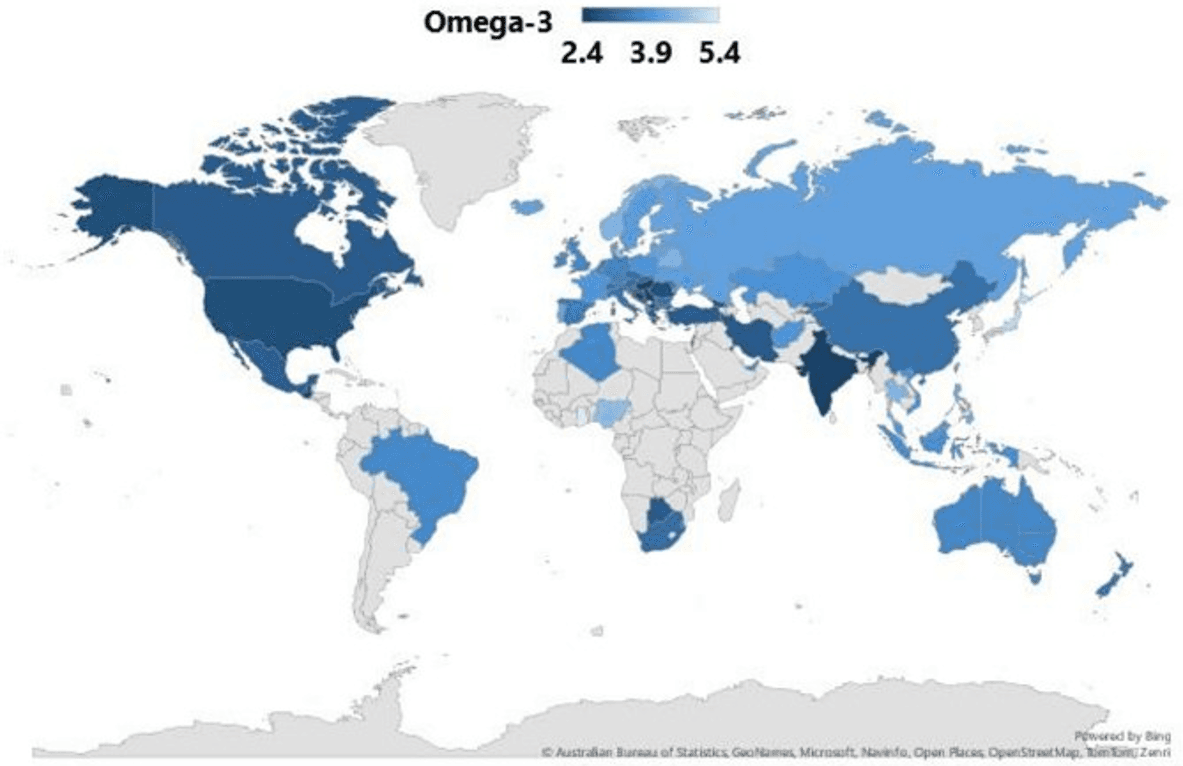
Global distribution of n-3 levels (omega-3) in countries with ≥ 35 samples (4)
Why Intake Alone May Not Be Enough
Fish oil supplements can raise blood levels of EPA and DHA, but higher levels alone don’t automatically translate into better inflammation control. For omega-3s to deliver their full benefit, the body still has to do several things effectively:
Absorb them properly
Incorporate them into cell membranes
Convert them into specialized pro-resolving mediators (SPMs)—the active compounds that actually help resolve inflammation
SPM production is frequently impaired in people with chronic illness, ongoing inflammation, high stress, nutrient deficiencies, or metabolic dysfunction. When the body can’t efficiently convert omega-3s into SPMs, simply taking more fish oil may not lead to meaningful clinical results. This may help explain why omega-3 intervention trials sometimes show inconsistent or modest benefits.
What Makes SPMs Different From Omega-3 Fish Oil?
Traditional omega-3 supplementation focuses on increasing intake of EPA and DHA, assuming higher levels will naturally lead to improved inflammatory control. However, SPMs function downstream of omega-3 fatty acids, and their effects are qualitatively different. SPMs are not anti-inflammatory in the conventional sense. Instead, they actively guide the immune system to resolve inflammation and restore tissue balance, without suppressing immune function. Preliminary evidence suggests SPM-enriched formulations may reduce inflammation and improve outcomes in obesity, atherosclerosis, infections, and chronic pain. (1)
SPMs have been shown to:
Improve the ability of immune cells to clear bacteria and debris
Reduce excessive activation of white blood cells and platelets
Reprogram immune cell signaling toward resolution rather than prolonged inflammation
This allows inflammation to shut down appropriately—without weakening the body’s ability to defend itself. That’s a major limitation of many pharmaceutical anti-inflammatories and even some nutraceutical approaches. By supplementing with SPMs directly, the body receives ready-to-use resolution signals, bypassing the need for enzymatic conversion that may be impaired in many individuals.
Reframing the Conversation Around Inflammation
Inflammation itself is not the problem—it is a vital part of the body’s healing process. The real issue arises when inflammation fails to resolve. While omega-3 fatty acids remain an essential nutritional foundation, they represent only the starting point in a much more complex biological process.
Specialized pro-resolving mediators (SPMs) offer a shift in how we think about inflammatory support. By directly supporting the body’s natural resolution pathways, SPMs may help address unresolved inflammation more effectively, particularly in individuals with chronic illness or persistent inflammatory states.
Citations:
1. Martindale R, Mundi MS, Waitzberg D, De Waele E, Scarcella M, Umbrello M, Calder PC, Dalli J, Puthucheary Z, van Zanten ARH. Integrating downstream mediators of Omega-3 fatty acids into enteral nutrition for improved patient care: An expert panel consensus. Clin Nutr. 2025 Nov 22;56:106529. doi: 10.1016/j.clnu.2025.11.014. Epub ahead of print. PMID: 41406625.
2. Grytten E, Laupsa-Borge J, Cetin K, Bohov P, Nordrehaug JE, Skorve J, Berge RK, Strand E, Bjørndal B, Nygård OK, Rostrup E, Mellgren G, Dankel SN. Inflammatory markers after supplementation with marine n-3 or plant n-6 PUFAs: A randomized double-blind crossover study. J Lipid Res. 2025 Apr;66(4):100770. doi: 10.1016/j.jlr.2025.100770. Epub 2025 Mar 8. PMID: 40058591; PMCID: PMC11999210.
3. Mensah, G, Arnold, N, Prabhu, S. et al. Inflammation and Cardiovascular Disease: 2025 ACC Scientific Statement: A Report of the American College of Cardiology. JACC. null2025, 0 (0) .https://doi.org/10.1016/j.jacc.2025.08.047
4. Torrissen M, Gisslevik E, Gundersen TE, Bolstad T, Eide O, Rizzo AM, Clayton P, Robertson C. Global variations in omega-3 fatty acid status and omega-6:omega-3 ratios: insights from > 500,000 whole-blood dried blood spot samples. Lipids Health Dis. 2025 Aug 9;24(1):260. doi: 10.1186/s12944-025-02676-6. PMID: 40783537; PMCID: PMC12335782.
Written by
My blog





